TMj and orofacial pain
The most common acute, or short-lasting, causes of TMJ (temporomandibular joint) and orofacial pain are related to dental issues and can be successfully relieved by a dentist or oral surgeon. Depending on the cause, primary care clinicians may also refer you to an otolaryngologist (ear, nose and throat doctor), neurologist, or pain specialist for treatment. Chronic facial pain, on the other hand, can be unilateral—meaning it occurs on one side of the head—or bilateral, meaning it occurs on both sides of the head. Chronic orofacial pain can be continuous or occur in episodes, or flashes.
Pain felt on one side of the face may be caused by a temporomandibular disorder (TMD), especially if it involves your chewing muscles. TMDs comprise a group of disabling conditions characterized by dysfunctions in the jaw muscles and/or the temporomandibular joint (that is the jaw joint that connects the lower jaw to the skull), with chronic orofacial pain as a typical feature. Depending on the severity of the disorder, TMD can affect your ability to speak, chew, swallow, and make facial expressions. Also included under the heading of TMD are disorders involving the jaw muscles. These may accompany the jaw joint problems or occur independently.
Depending on the severity of the disorder, TMD can affect your ability to speak, chew, swallow, and make facial expressions. Also included under the heading of TMD are disorders involving the jaw muscles. These may accompany the jaw joint problems or occur independently.
Causes of TMJ Disorders
The TMJ is complex, with many associated muscles, tissues, and facial nerves. For example, 150,000 people are diagnosed with trigeminal neuralgia (facial pain) every year. While the disorder can occur at any age, and is more common in women, it is most common in those over age 50, according to the American Association of Neurological Surgeons. Also, many of the ears’ elaborate mechanisms are close by. Because the TMJ is so complex, changes in any one of these parts of the TMJ can lead to development of a TMD.
Possible Causes of TMDs:
A disorder in the articular disc between the skull and jawbone: The articular disc helps keep jaw movement smooth.
Arthritis and/or inflammation in the TMJ: Cartilage in the TMJ can become damaged by arthritis.
Constantly chewing gum: Chewing gum too often as well as other environmental factors may contribute to a TMJ disorder.
Grinding your teeth or clenching your jaw: Tension in the jaw muscles can lead to a TMD.
Hormones: TMDs are more common in women than in men (especially women in their childbearing years). Researchers think there may be a link between female sex hormones and TMDs.
Jaw injury: A jaw injury (even a minor one) can lead to a TMD.
Your genes: For example, if your mom has a TMD, you’re more prone to developing one, too.
It’s important to note that not everyone who is at risk for a TMD will actually develop one. For example, many people who grind their teeth may never get a TMD; on the other hand, you can get a TMD even if you don’t grind your teeth or have jaw pain.
Although the cause of TMDs isn’t always clear, your physician or dentist can help you address any questions you have about the possible causes of TMDs.
Other Health Conditions With TMD
You may experience other health conditions along with your TMD. People with chronic fatigue syndrome, fibromyalgia, sleep disturbances, and arthritis often experience TMD, too. TMJ experts do not know if all of these conditions share common causes.
Your TMD may challenge your physicians. While the symptoms are somewhat obvious, actually sorting out TMDs from a number of other conditions is complex. With a moderate to complex case, it is hard to know which treatments will be ideal for your situation.
You and your clinician many need to exercise patience, as you use trial and error with the various treatments, until you find one or more beneficial treatments.
TMJ Case Study
Patient had history of injury to his face which caused dropping of jaw on even rest position. He came with a belt around his jaw anchored with his head. On removal of the belt his lower jaw opened and was unable to close on his own.



The lower jaw had to be manipulated to force close his mouth. On his CBCT scan it was noticed that his lower jaw moved too forward and was unable to close.
He was advised and the surgery was performed to remove the condyle of lower jaw post operative. His mouth was closed with wires for one week.
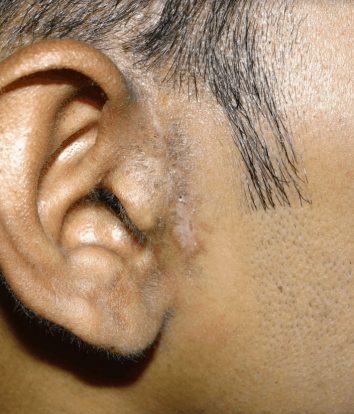
Later he was given elastics for 2 weeks. All wires and elastics were removed at the end of three weeks post surgery. The post operation incision scar very insignificant is seen.

For more information regarding management of TMJ related pain click here:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5859913/
Check out our other popular pages:
